| Journal of Endocrinology and Metabolism, ISSN 1923-2861 print, 1923-287X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Endocrinol Metab and Elmer Press Inc |
| Journal website http://www.jofem.org |
Case Report
Volume 6, Number 4, August 2016, pages 129-131
Fatal Pituitary Tumor Apoplexy Presenting With Behavioral Disorder
Francisco Tortosaa, b, c, Santiago Ortiza
aDepartment of Pathology, Centro Hospitalar Lisboa Norte, EPE - Hospital de Santa Maria, Av. Prof. Egas Moniz, 1649-035 Lisbon, Portugal
bDepartment of Medicine/Endocrinology, Hospital Sant Pau, Universitat Autonoma de Barcelona (UAB), Pare Claret 167, 08025 Barcelona, Spain
cCorresponding Author: Francisco Tortosa, Department of Pathology, CHLN, EPE - Hospital de Santa Maria, Av. Prof. Egas Moniz, 1649-035 Lisbon, Portugal
Manuscript accepted for publication August 17, 2016
Short title: Fatal Pituitary Tumor Apoplexy
doi: http://dx.doi.org/10.14740/jem363w
| Abstract | ▴Top |
Pituitary apoplexy (PA) is a rare but potentially fatal ischemic or hemorrhagic phenomenon, with an annual incidence around 1.2 per million. It is often misdiagnosed because most patients have subclinical pituitary adenomas and its presentation can be confused with neurological or, very rarely, psychiatric processes. Here, we present a 31-year-old man, with history of hypertension and chronic renal disease on hemodialysis of unknown etiology, admitted in the Department of Psychiatry of our Hospital with altered behavioral symptoms. Neuroimaging studies showed an increase of the pituitary gland due to an intraparenchymatous lesion. He was found dead on his room floor. In the autopsy, we observed a pituitary increased in weight and size, which in sagittal section showed an extensive hemorrhagic area located in the anterior lobe. Histological examination revealed a 9 mm adrenocorticotrophic adenoma (ACTH-secreting adenoma), with an extensive intratumoral hemorrhage. PA is often a difficult diagnosis, since it can mimic other clinical situations. Clinicopathologic effects of PA are caused by a rapid increase in the size of the contents of the pituitary fossa and the subsequent rise of intrasellar pressure, with additional pressure on the hypothalamus and midbrain. This would possibly explain the alteration of vital functions and consciousness. Pituitary hemorrhage normally produces an acute stroke which causes characteristic symptoms; the extremely rare case that we present exemplifies how it may also have subclinical/insidiously course for days. To our knowledge, this is the first time to report that a so obvious macroscopic image of post-mortem pituitary with this rare disease.
Keywords: Pituitary apoplexy; Pituitary adenoma
| Introduction | ▴Top |
Pituitary apoplexy (PA) is a rare but potentially fatal ischemic or hemorrhagic phenomenon. It is often misdiagnosed because most patients have subclinical pituitary adenomas and its presentation can be confused with neurological or, very rarely, psychiatric processes. Clinically, it has been defined as the sudden onset of symptoms such as intense headache (retro-orbital location), nausea, vomiting, visual disturbances, paralysis of cranial nerves and/or altered state of consciousness with radiological evidence of a hemorrhagic pituitary infarction [1]. The mean age of presentation is 51 - 52 years, being more frequent in males (60%) [2, 3]. Classic PA is a rare disease with an annual incidence around 1.2 per million [4]. Its acute form, described only in 1-2% of the pituitary adenomas, can be dramatic, coursing with severe neurologic deficits, coma and even death. Sudden death by PA without association of the most common symptoms, an extraordinary event, has rarely been reported [5, 6].
| Case Report | ▴Top |
We report a black 31-year-old man from Cape Verde, with history of hypertension and chronic renal disease (unknown etiology) on hemodialysis. He was admitted in the Department of Psychiatry of our Hospital with altered behavioral symptoms of unknown etiology. Emergency head computed tomography did not identify focal lesions with mass effect, acute intracranial hematomas or territorial hypodensities suggestive of acute ischemia. Head magnetic resonance imaging showed an increased height of the pituitary gland due to an intraparenchymatous lesion, hypointense on T1 and hyperintense on T2, to deserve merit a more targeted study. During his internment, he was diagnosed of hypercortisolism and Cushing’s disease with neurosurgical indication. With high in hemodialysis program, he was readmitted in the Gastroenterology Service by an acute pancreatitis. He was found on his room floor in cardiac arrest and after appropriate resuscitation maneuvres, the death was verified.
In the autopsy, we observed a pituitary increased in weight and size, which in sagittal section showed an extensive hemorrhagic area located in the anterior lobe (Fig. 1). Histological examination revealed a 9 mm adrenocorticotrophic adenoma (ACTH-secreting adenoma), with extensive intratumoral hemorrhage.
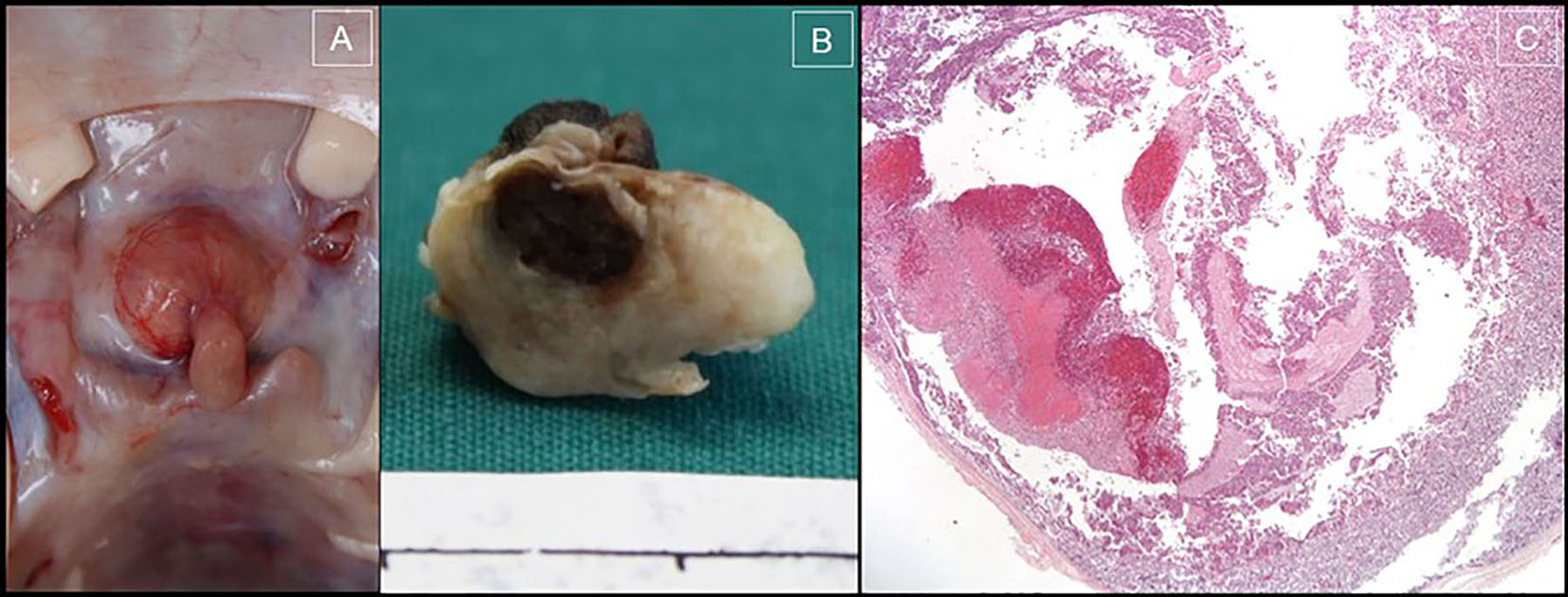 Click for large image | Figure 1. (A) Enlargement of the pituitary gland in the sella turcica. (B) Sagittal section of the pituitary gland (fixed in 10% buffered formaldehyde), in the anterior lobe, an extensive hemorrhagic area is observed. (C) Photomicrograph of pituitary adenoma with hemorrhagic and cystic areas (H&E, × 20). |
| Discussion | ▴Top |
PA is often a difficult diagnosis, since it can mimic other clinical situations. It may cause any pituitary hormone deficiency, requiring prompt treatment, once the abrupt deficit of ACTH and consequently of cortisol, it may cause serious complications and potentially death [7]. It may happen in two ways: acute (appears abruptly in 24 - 48 h and it is considered a life-threatening neuroendocrine emergency) or silent/subclinical (more insidious evolution, with mild or no clinical manifestations, it is usually produced by intratumoral hemorrhage) [7].
The precise pathogenic mechanism leading to the PA is not well known. Many theories have been postulated. Randeva et al (1999) conducted a retrospective study with the objective to establish the clinical presentation, predisposing factors, treatment and evolution of patients with PA [1]. They concluded that the most common symptom is headache and that hypertension can be an important predisposing factor (our patient was hypertensive). In other retrospective studies, we have observed that PA is an uncommon complication of adenomas, around 4-5% [8, 9]. Clinicopathological consequences of PA are caused by a rapid increase in the size of the pituitary fossa and the consequent rise of intrasellar pressure [10]. As a result of this upward expansion of the pituitary gland, it produces a compression of the optic chiasm, resulting in alterations of the visual field, specifically a bitemporal hemianopsia. Less frequently, the additional pressure exerted on the hypothalamus and midbrain could explain the alteration of vital functions and consciousness [11], once it is here where the secretory functions are regulated, the water balance is controlled; it regulates food intake, body temperature and influences the state of consciousness, sleep, emotions and behavior. Thus, it follows the panhypopituitarism, symptoms such as polydipsia, hyperphagia and poikilothermia, and cognitive and behavioral symptoms such as aggression, depression, irritability, mental confusion and memory commitment, which may be clinical manifestations of hypothalamic involvement.
The relationship between hypercortisolism and psychiatric disorders, which have already been described: depression, mania, anxiety and impaired memory and attention, is well documented [12, 13].
Patients with PA can occur in different clinical specialties departments, which often lead to difficulties and delays in diagnosis. Although computed tomography is most commonly used in research of acute neurological disorders, it is not sensitive in the diagnosis of PA, because it identifies the presence of hemorrhage or infarction within this gland only in 21-28% of cases. Magnetic resonance imaging confirms the diagnosis in over 90% of cases, being the method of choice [1, 14].
There is no consensus on the optimal treatment of PA [7]. The immediate treatment of fluids, electrolytes balance and the hydrocortisone replacement will be the priorities; the conservative treatment of patients with mild and stable neuro-ophthalmologic symptoms is probably safe. Patients with severely decreased visual acuity, decreased level of consciousness and hypothalamic alteration, should be submitted to an emergency neurosurgical decompression.
Conclusion
PA is a rare but potentially fatal condition. The differential diagnosis is broad, although an extensive pituitary hemorrhage normally produces an acute stroke that causes characteristic symptoms. The case that we present, clearly exemplifies, how it may also have subclinical/insidiously course for days, with minimal (if any) clinical symptoms. To other less common symptoms or, an atypical presentation, which can delay the diagnosis and management of the patient, the clinician must be alert to this diagnostic possibility. The case describes an uncommon complication in a microadenoma; to our knowledge, this is the first time to report that a so obvious macroscopic image of post-mortem pituitary with this rare disease.
Acknowledgments
We thank Ana Raquel Henriques for help with the translation into English.
Conflicts of Interest
None.
Funding Source
None.
| References | ▴Top |
- Randeva HS, Schoebel J, Byrne J, Esiri M, Adams CB, Wass JA. Classical pituitary apoplexy: clinical features, management and outcome. Clin Endocrinol (Oxf). 1999;51(2):181-188.
doi - Semple PL, Webb MK, de Villiers JC, Laws ER, Jr. Pituitary apoplexy. Neurosurgery. 2005;56(1):65-72; discussion 72-63.
- Ayuk J, McGregor EJ, Mitchell RD, Gittoes NJ. Acute management of pituitary apoplexy - surgery or conservative management? Clin Endocrinol (Oxf). 2004;61(6):747-752.
doi pubmed - Nielsen EH, Lindholm J, Bjerre P, Christiansen JS, Hagen C, Juul S, Jorgensen J, et al. Frequent occurrence of pituitary apoplexy in patients with non-functioning pituitary adenoma. Clin Endocrinol (Oxf). 2006;64(3):319-322.
doi pubmed - Sun T, Liu L, Sunnassee A, Zhuo L, Zhu S. Sudden death in custody due to pituitary apoplexy during long restriction in a sitting position: a case report and review of the literature. J Forensic Leg Med. 2013;20(7):812-815.
doi pubmed - Shields LB, Balko MG, Hunsaker JC, 3rd. Sudden and unexpected death from pituitary tumor apoplexy. J Forensic Sci. 2012;57(1):262-266.
doi pubmed - Catala M, Pico A, Tortosa F, Varela C, Gilsanz A, Lucas T, et al. Clinical practice guideline for the diagnosis and treatment of pituitary apoplexy. Endocrinol Nutr. 2006;53:19-24.
- Tortosa F, Webb SM. Atypical pituitary adenomas: 10 years of experience in a reference centre in Portugal. Neurologia. 2016;31(2):97-105.
doi pubmed - Tortosa F, Ortiz S. Histopathological features of postmortem pituitaries: a retrospective analysis. Rev Assoc Med Bras. (Article In press).
- Zayour DH, Selman WR, Arafah BM. Extreme elevation of intrasellar pressure in patients with pituitary tumor apoplexy: relation to pituitary function. J Clin Endocrinol Metab. 2004;89(11):5649-5654.
doi pubmed - Watt A, Pobereskin L, Vaidya B. Pituitary apoplexy within a macroprolactinoma. Nat Clin Pract Endocrinol Metab. 2008;4(11):635-641.
doi pubmed - Sonino N, Fava GA. Psychiatric disorders associated with Cushing's syndrome. Epidemiology, pathophysiology and treatment. CNS Drugs. 2001;15(5):361-373.
doi pubmed - Kiraly SJ, Ancill RJ, Dimitrova G. The relationship of endogenous cortisol to psychiatric disorder: a review. Can J Psychiatry. 1997;42(4):415-420.
pubmed - Sibal L, Ball SG, Connolly V, James RA, Kane P, Kelly WF, Kendall-Taylor P, et al. Pituitary apoplexy: a review of clinical presentation, management and outcome in 45 cases. Pituitary. 2004;7(3):157-163.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Endocrinology and Metabolism is published by Elmer Press Inc.