| Effect of Vitamin D on Type 1 Diabetes |
| Immune modulator | Presence of vitamin D receptors (VDR) on antigen presenting cells (macrophages and dendritic cells) and activated T-Lymphocytes.
Vitamin D (VD) downregulates antigen presentation and expression of co-stimulatory molecule by dendritic cells, thus inhibiting the production of proinflammatory cytokines.
VD also promotes the induction of regulatory T-lymphocytes and the production of anti-inflammatory cytokine IL-4. |
| Protection of beta-cell | VD prevents beta-cell damage caused by pro-inflammatory cytokines (IL-1β and IFN-γ) by inhibiting the synthesis of inflammatory cytokines. |
| Effect of Vitamin D on Type 2 Diabetes |
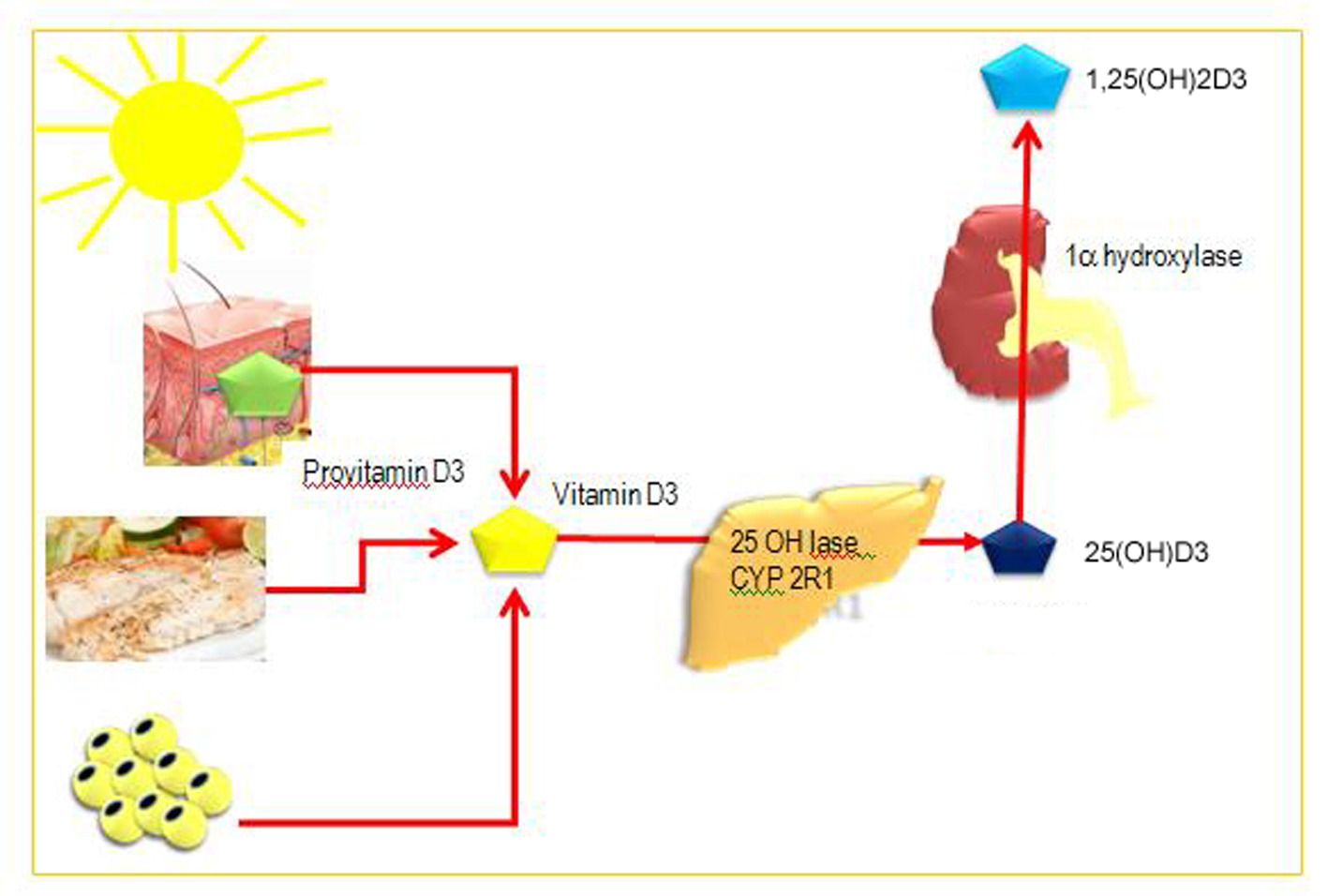
| Effect of vitamin D on insulin secretion | Presence of vitamin D receptor in pancreatic beta-cells and expression of 1,25 hydroxylase enzyme in pancreatic beta-cells suggest a role of VD in insulin secretion.
Alterations in calcium flux can have adverse effects on insulin secretion, a calcium-dependent process.
VD improves insulin secretion and glucose tolerance through regulation of the calcium levels. VD may induce insulin secretion indirectly by increasing the intracellular calcium concentration.
Subsequently VD may mediate the activation of calcium dependent endopeptidases which facilitate the conversion of proinsulin to insulin. |
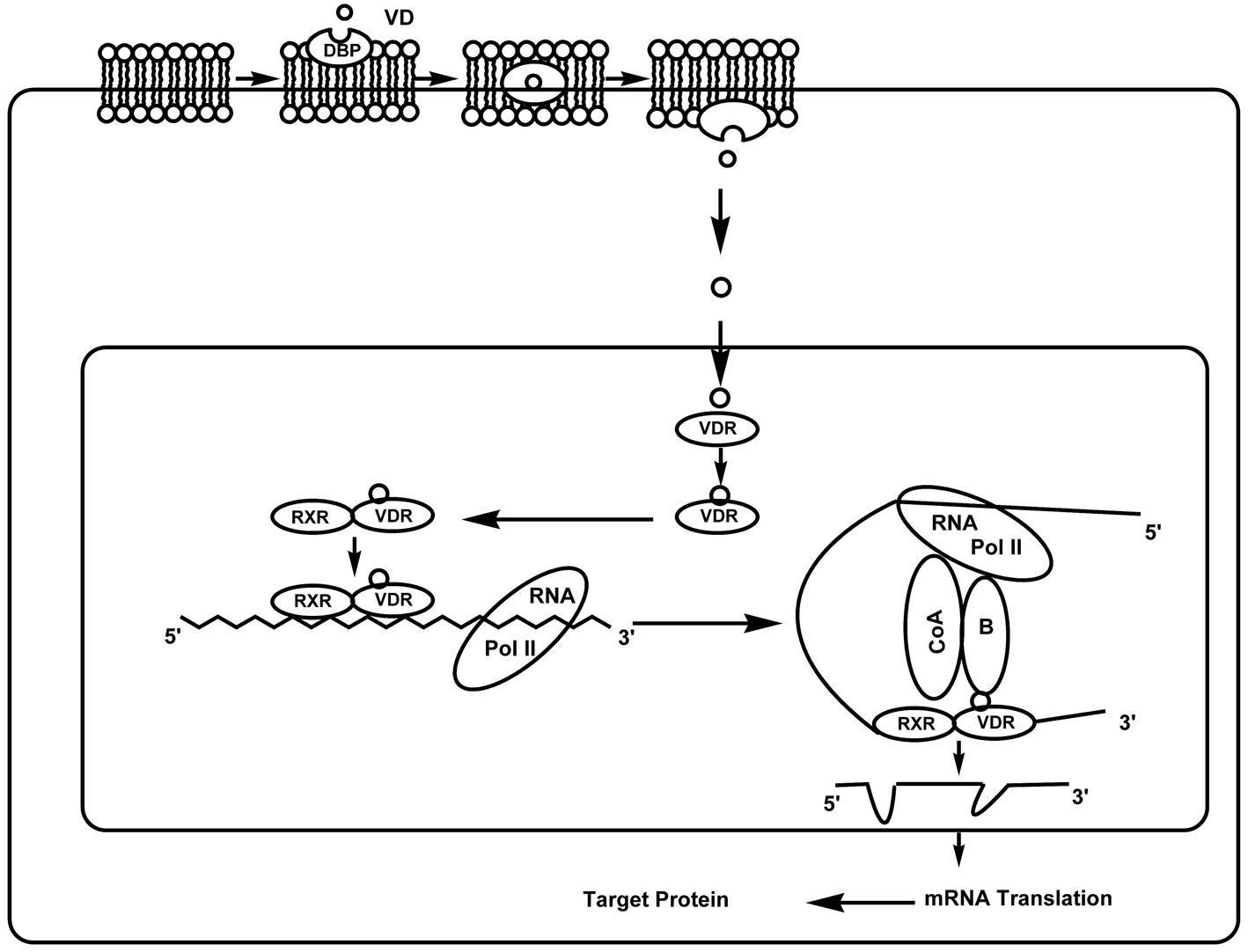
| Effect of vitamin D on insulin action | VD mediates the transcriptional activation of human insulin gene (Vitamin D Responsive Element [VDRE] is present in human insulin gene promoter region) and also stimulates the expression of insulin receptor thereby enhancing insulin responsiveness for glucose transport.
VD may have a beneficial effect on insulin action indirectly via its role in regulating extracellular calcium levels, as calcium is essential for insulin mediated processes in insulin responsive tissues. |
| Effect of vitamin D on cytokines | VD may improve insulin sensitivity and promote beta-cell survival by modulating the effects of cytokines.
VD interacts with vitamin D response elements in the promoter region of cytokine genes to interfere with nuclear transcription factors implicated in cytokine generation and action.
Vitamin D can downregulate the activation of NF-kB, which is an important regulator of genes encoding pro-inflammatory cytokines implicated in insulin resistance.
Vitamin D interferes with cytokine generation by upregulating expression of calbindin, a cytosolic calcium-binding protein found in many tissues including pancreatic beta-cells. Calbindin has been shown to protect against cytokine-induced apoptosis that may occur after a rise in cytosolic free calcium [Ca2+]I. |