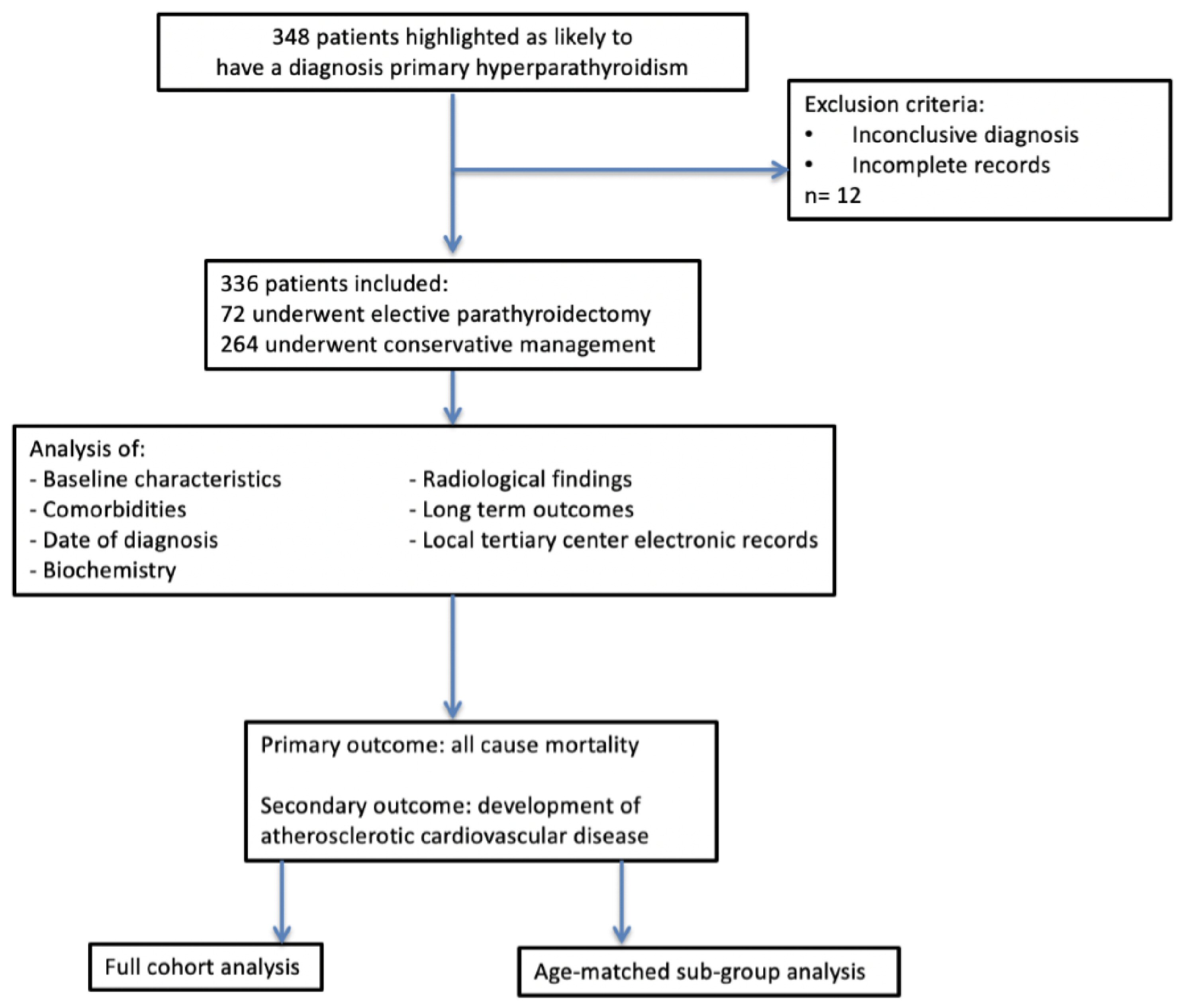
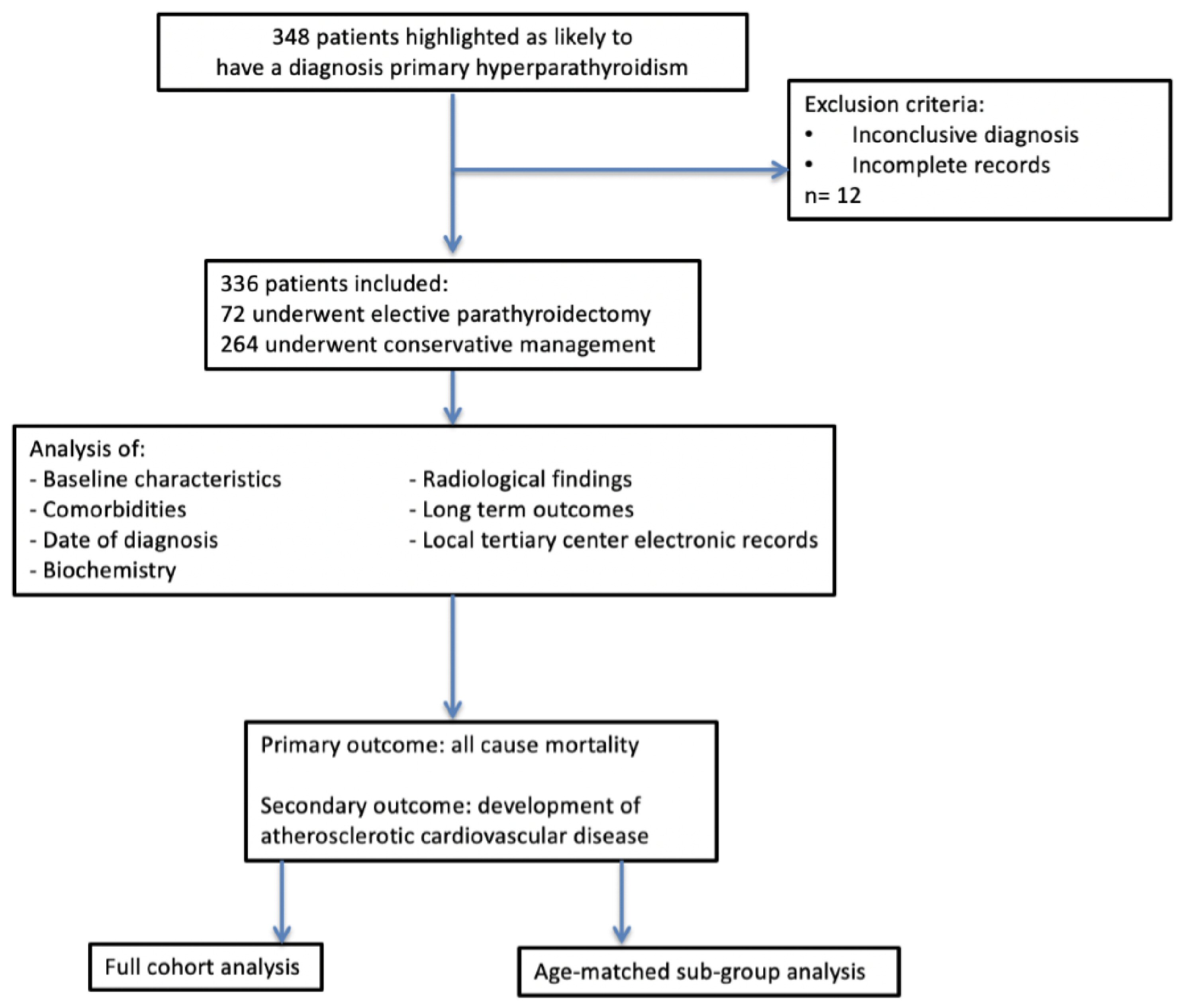
Figure 1. Methodology.
| Journal of Endocrinology and Metabolism, ISSN 1923-2861 print, 1923-287X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Endocrinol Metab and Elmer Press Inc |
| Journal website http://www.jofem.org |
Original Article
Volume 9, Number 4, August 2019, pages 95-107
Primary Hyperparathyroidism: Comparing Cardiovascular Morbidity and Mortality in Patients Treated With Parathyroidectomy Versus Conservative Management
Figures
Tables
| Conservative | Surgical | P value | |
|---|---|---|---|
| Statistical tests: Mann-Whitney, unpaired t-test. *Denotes significance (P < 0.05). S.Ca: serum corrected calcium; PTH: parathyroid hormone. | |||
| Number of patients | 264 | 72 | - |
| Male/female | 59:277 | 11:61 | - |
| Mean age in years (range) | 68.7 (26 - 90) | 56.8 (33 - 84) | 0.001* |
| Mean S.Ca at diagnosis (mmol/L) | 2.70 | 2.72 | 0.498 |
| Mean PTH at diagnosis (pg/mL) | 11.4 | 16.5 | 0.034* |
| Conservative | Surgical | P value | |
|---|---|---|---|
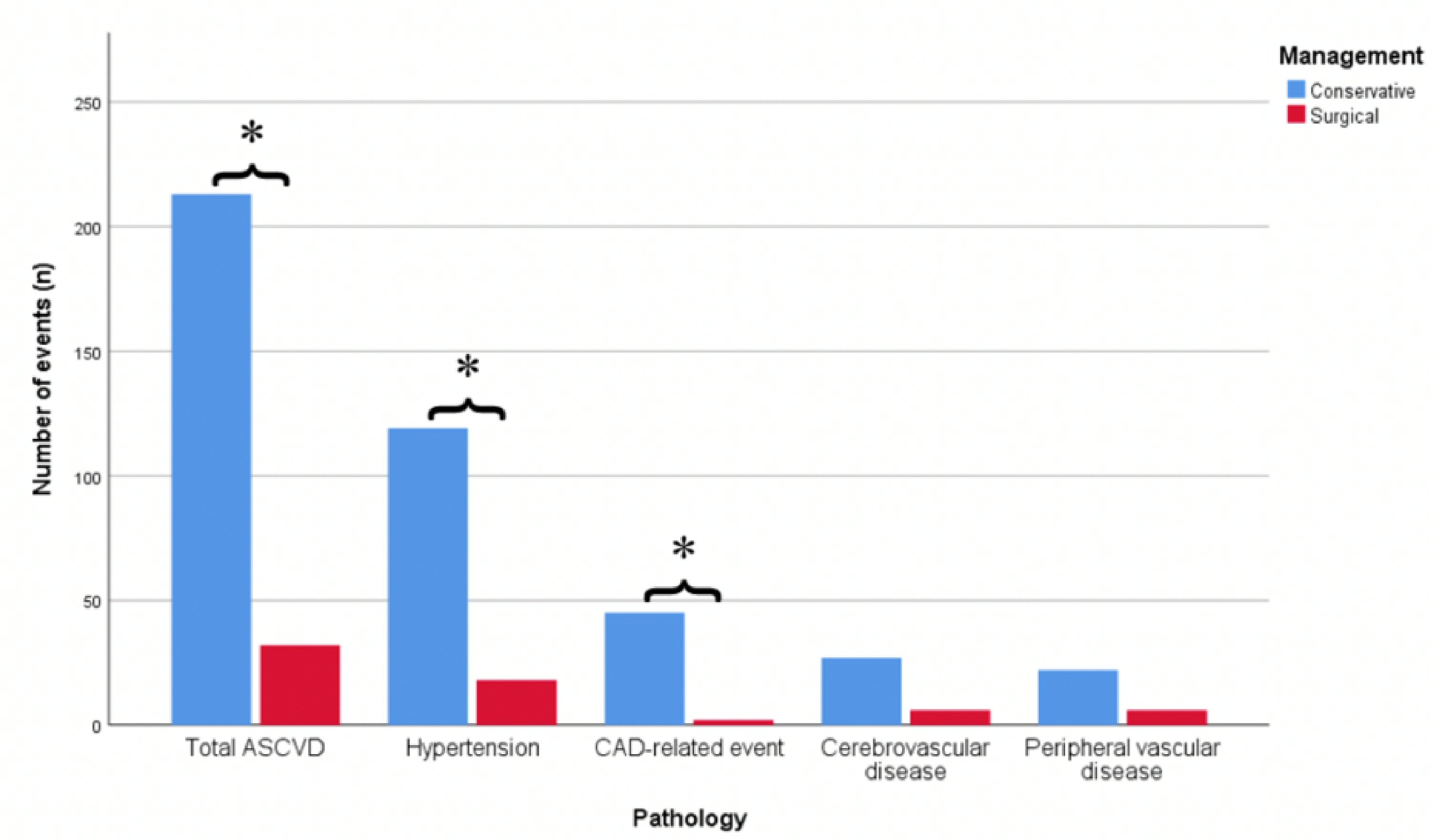
| Statistical tests: Mann-Whitney, Fisher’s test. *Denotes significance (P < 0.05). Percentage is not stated for total ASCVD as single patient may have had multiple events. CAD: coronary artery disease; ASCVD: atherosclerotic cardiovascular disease. | |||
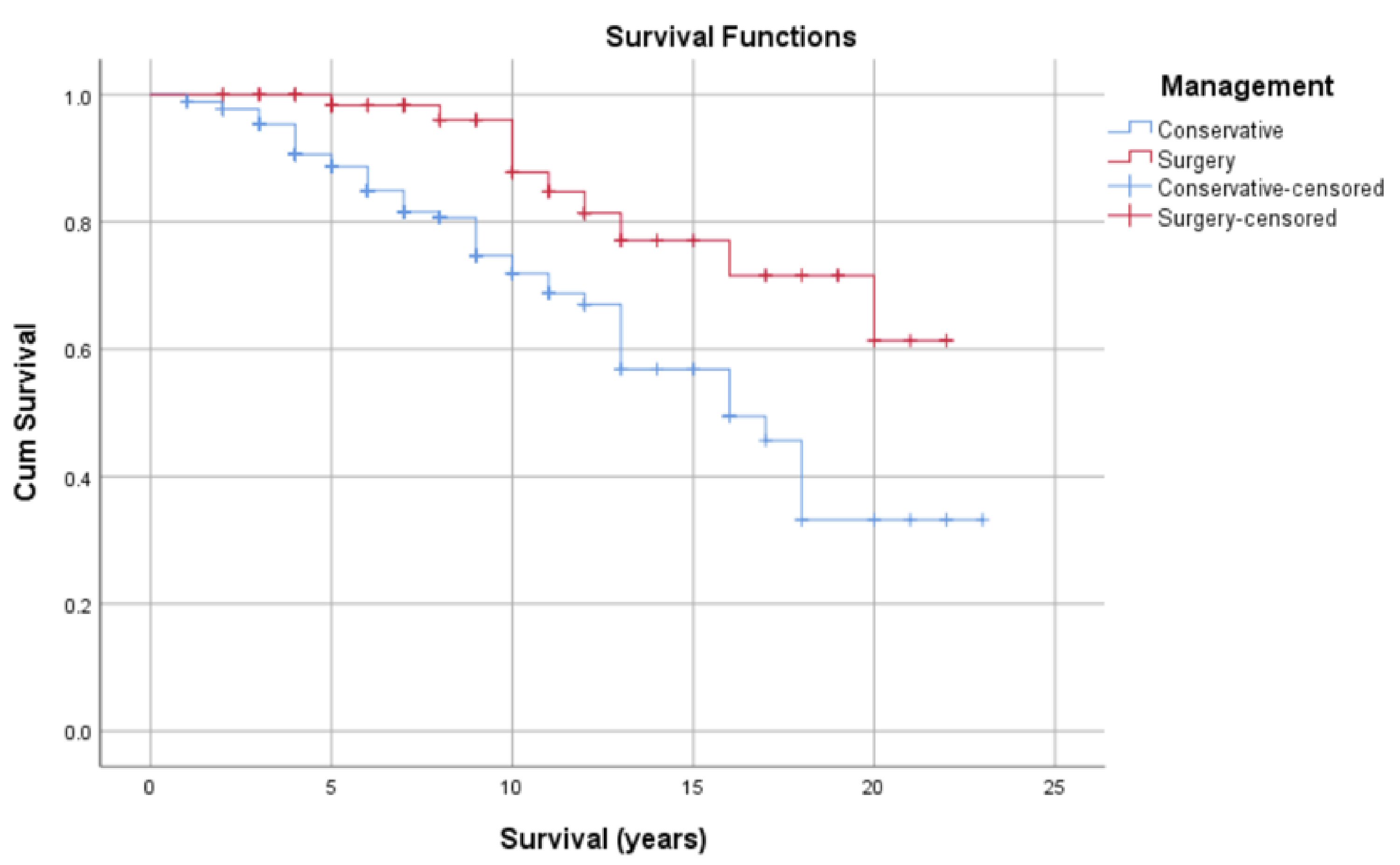
| Mortality | 62 (23.4%) | 10 (13.8%) | 0.104 |
| Hypertension | 119 (45.2%) | 18 (25%) | 0.002* |
| CAD-related events | 45 (17.1%) | 2 (2.8%) | 0.001* |
| Cerebrovascular disease | 27 (10.2%) | 6 (8%) | 0.824 |
| Peripheral vascular disease | 22 (8%) | 6 (8%) | 1.00 |
| Total ASCVD events | 213 | 32 | 0.001* |
| Duration of clinic follow-up in years (range) | 7.25 (0.5 - 23) | 2.42 (0.3 - 13) | 0.001* |
| B (coefficient) | SE | Sig. | OR (Exp(b)) | 95% CI for OR | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| *Denotes significance (P < 0.05). CI: confidence interval; OR: odds ratio. | ||||||
| Age | 0.033 | 0.010 | 0.001* | 1.033 | 1.014 | 1.053 |
| Surgery | -0.729 | 0.330 | 0.027* | 0.482 | 0.253 | 0.921 |
| Constant | -2.816 | 0.747 | 0.000 | 0.060 | ||
| Conservative (age-matched subgroup) | Surgical | P value | |
|---|---|---|---|
| Statistical tests: Mann-Whitney, unpaired t-test. *Denotes significance (P < 0.05). S.Ca: serum corrected calcium; PTH: parathyroid hormone. | |||
| Number of patients | 72 | 72 | - |
| Male/female | 11:61 | 11:61 | - |
| Mean age at diagnosis | 59.8 (26 - 87) | 56.8 (33 - 84) | 0.139 |
| Mean age now/age at death (years) | 66.3 (30 - 96) | 65.9 (40 - 95) | 0.865 |
| Mean S.Ca at diagnosis (mmol/L) | 2.67 | 2.73 | 0.221 |
| Mean PTH at diagnosis (mmol/L) | 10.07 | 15.1 | 0.018* |
| Conservative (age-matched subgroup) | Surgical | P value | |
|---|---|---|---|
| Statistical tests: Chi-squared, Fisher’s test. *Denotes significance (P < 0.05). Percentage is not stated for total ASCVD as single patient may have had multiple events. CAD: coronary artery disease; ASCVD: atherosclerotic cardiovascular disease. | |||
| Mortality | 6 (8.3%) | 10 (13.8%) | 0.427 |
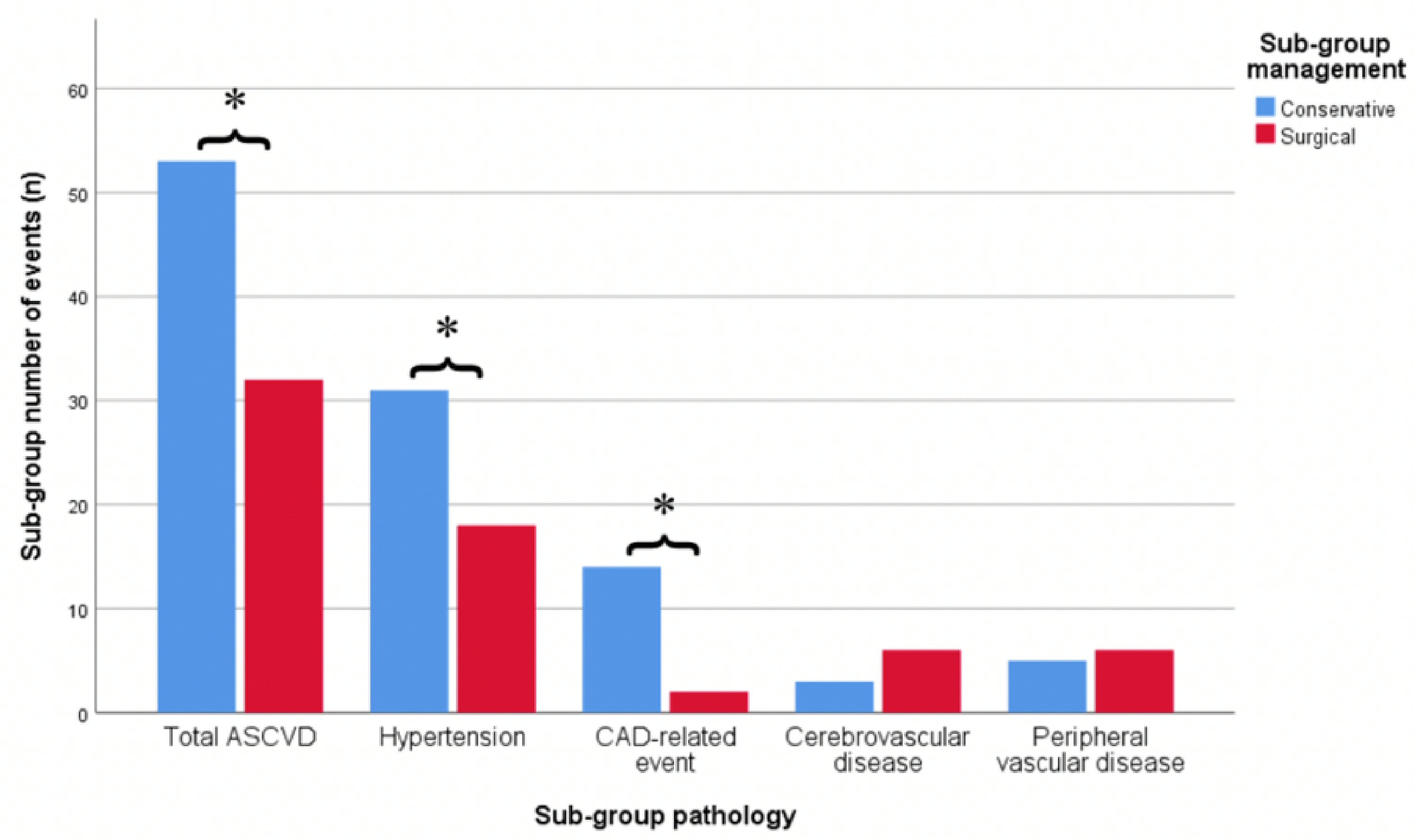
| Hypertension | 31 (43%) | 18 (25%) | 0.022* |
| CAD-related events | 14 (19%) | 2 (2.8%) | 0.002* |
| Cerebrovascular disease | 3 (4%) | 6 (8%) | 0.299 |
| Peripheral vascular disease | 5 (7%) | 6 (8%) | 0.089 |
| Total ASCVD | 53 | 32 | 0.001* |
| B (coefficient) | SE | Sig. | OR (Exp (b)) | 95% CI for OR | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| CI: confidence interval; OR: odds ratio. | ||||||
| Surgery | -1.249 | 0.357 | 0.001* | 0.287 | 0.142 | 0.578 |
| Constant | -0.223 | 0.237 | 0.347 | 1.250 | ||
| Study authors (reference) | Design | Number of participants | Results | Comments |
|---|---|---|---|---|
| ARR: aldosterone to renin ratio; BP: blood pressure; CKD: chronic kidney disease; EPATH: “Eplerenone in Primary Hyperparathyroidism” trial; HTN: hypertension; LVH: left ventricular hypertrophy; PTH: parathyroid hormone; MESA: Multi-Ethnic Study of Atherosclerosis; PHPT: primary hyperparathyroidism; SBP: systolic blood pressure. | ||||
| Brown et al, 2015 [44] | Cross-sectional analysis of MESA participants without PHPT or CKD | 5,668 | Higher serum aldosterone was associated with higher serum PTH. Higher PTH levels were observed in patients with HTN. The use of RAAS inhibitors was associated with lower PTH levels. | Large diverse population. Association shown, causation not clear. Led onto EPATH study. |
| Heyliger et al, 2009 [28] | Retrospective review of patients undergoing parathyroidectomy for PHPT or thyroidectomy for non-toxic thyroid disease | 464 | Significant decrease in BP (< 10 mm Hg) after parathyroidectomy in patients with preoperative hypertension. | Large sample size. Retrospective design. Single BP measurements taken pre- and post-operatively. Patients who had preoperative alterations in BP medications were excluded. |
| Nainby-Luxmoore et al, 1982 [25] | Case control study; patients with PHPT undergoing parathyroidectomy and matched surgical controls | 248 | Mean BP in patients with PHPT was higher than matched controls. This difference was no longer observed at discharge. | Difference persisted when controlled for renal function. |
| Stefenelli et al, 1997 [29] | Prospective study; baseline LV mass pre- and post- elective parathyroidectomy on patients with PHPT | 119 | Regression of LVH after 41 months of parathyroidectomy. LVH reduction was independent of changes in BP. | LV mass measured using echocardiography; potential for operator variability in measurements. |
| Verheyen et al, 2016 [27] | Cross-sectional analysis of the EPATH trial, studied association between PTH levels and nocturnal hypertension | 136 | PTH levels did not correlate with nocturnal hypertension. Significant relationship between ARR and nocturnal SBP in patients with high PTH. | Small sample size, single-center study. Daytime SBP readings not assessed. |
| Yao et al, 2016 [26] | Prospective observational study on health population, median follow-up of 6 years, monitored for development of HTN | 7,504 | Raised PTH levels were associated with an increased risk of development of hypertension. | Large sample size. Participants with pre-existing ASCVD at baseline excluded. PTH only measured on one occasion. |
| Study authors (reference) | Design | Number of participants | Results | Comments |
|---|---|---|---|---|
| 25(OH)D: 25-hydroxyvitamin D; Aix: augmentation index; AVCA: aortic valve calcification area; CVD: cardiovascular disease; HF: heart failure; HTN: hypertension; IMT: intima media thickness; LVM: left ventricular mass; PHPT: primary hyperparathyroidism; PTH: parathyroid hormone; PWA: pulse wave analysis; PWV: pulse wave velocity; MRI: magnetic resonance imagining. | ||||
| Bansal et al, 2014 [39] | Cross-sectional analysis of participants of MESA. Healthy cohort without ASCVD. | 6,459 | Higher PTH associated with higher levels of incident HF (hazard ratio: 1.96). Higher PTH associated with higher LVM (11g mean difference). | Multi-ethnic large population. Cardiac MRI used to quantify LVM. Single baseline measurement of PTH and 25(OH)D. |
| Dalberg et al, 1996 [40] | Prospective case control study; patients with PHPT undergoing parathyroidectomy and matched controls undergoing thyroidectomy. | 67 | Higher BP, left atrial diameter and diastolic dysfunction in PHPT patients when compared to controls. Reduced cardiac calcifications post parathyroidectomy. | Prospective design. Small sample size. Use of echocardiography associated with potential of operator bias. |
| Iwata et al, 2012 [10] | Case-control study; patients with PHPT and matched controls (further analysis of Walker 2009 cohort). | 100 | AVCA positively associated with PTH level; no difference in peak transaortic pressure gradient. | Control group had more cardiovascular risk factors. Use of echocardiography associated with potential operator bias. AVCA is an indirect marker for ASCVD. |
| Rosa et al, 2011 [31] | Case-control study; 28 patients with PHPT and hypertension, 16 with PHPT without HTN, 28 essential HTN patients, 18 healthy controls. | 90 | PWV significantly higher in patients with PHPT and HTN compared with those with essential HTN. Surgery significantly decreased systolic BP and PWV. | Well matched baseline characteristics. Singular BP measurements (not ambulatory). |
| Rubin et al, 2005 [32] | Case-control study; patients with mild PHPT and matched healthy controls. | 173 | PHPT was an independent predictor of increased arterial stiffness. PTH levels directly correlated with arterial stiffness (measured by AIx) | Small proportion of cases compared to controls. Surrogate marker of arterial stiffness used. |
| Schillaci et al, 2011 [34] | Case-control study; patients with mild PHPT and matched healthy controls. | 72 | Aortic PWV was significantly higher among PHPT patients. Aortic PWV decreased after surgery. Association remained significant when controlled for BP. | Patients with pre-existing hypertension, CV disease excluded. PWV is a surrogate marker. |
| Smith et al, 2000 [33] | Case-control study; patients with mild PHPT and matched healthy controls. | 42 | PWA showed augmentation in PHPT group significantly higher than controls. Central aortic systolic pressure also elevated. | PWA indirect measure of vascular stiffness (surrogate marker of clinical disease). Small sample size. |
| Vestergaard et al, 2003 [41] | Case-control study, patients with PHPT undergoing parathyroidectomy compared to matched controls. | 2,695 | Increased incidence of acute MI in PHPT patients up to 10 years prior and 1 year post surgery. Increased risk of HTN and HF, which did not resolve by 1 year post surgery. | Large sample size. Historical follow-up. |
| Walker et al, 2009 [35] | Case-control study; patients with PHPT and matched healthy controls. | 1,040 | IMT higher in PHPT patients. Odds of abnormal carotid stiffness increased for every 10 pg/mL increase in PTH. | Small proportion of cases compared to controls. Control group was not well matched with respect to cardiovascular risk factors. |
| Wannamethee et al, 2014 [38] | Prospective observational study of healthy cohort (British Regional Heart Study); 13-year follow-up. | 3,731 | Raised PTH at baseline was associated with increased CV risk factors. Higher risk of incident HF with elevated PTH levels (hazard ratio: 1.66) independent of HTN, renal dysfunction, calcium and vitamin D levels. | Large sample size. Study based on older, predominately white, male population. Doctor diagnosed HF, echo not available in all patients. |
| Study authors (reference) | Design | Number of participants | Results | Comments |
|---|---|---|---|---|
| CI: confidence interval; CVD: cardiovascular disease; PHPT: primary hyperparathyroidism; RR: relative risk. | ||||
| Hedback et al, 1991 [45] | Retrospective observational study on patients with PHPT who had undergone parathyroidectomy; 13-year follow-up. | 896 | Increased risk of death in patients who had undergone parathyroidectomy when compared to the general population. This effect was more marked in those operated on in earlier calendar years, and in older patients. | Only included patients who underwent surgery. Historical study, therefore, caution should be applied if extrapolating these results to current surgical practice. |
| Lundgren et al, 2001 [9] | Observational case-control study; patients with hypercalcemia and matched normocalcemic controls. | 516 | Hypercalcemia was independently associated with increased CV mortality. There were also higher PTH levels in cases versus controls. | Large sample size, follow-up over 20 years. Association shown but cannot comment on causality. |
| Nilsson et al, 2002 [44] | Retrospective cohort study; patients with PHPT who had undergone parathyroidectomy. | 10,995 | In earlier calendar years increased risk of death following surgery. In those operated in later calendar years mortality did not differ from normal population. Principle causes of mortality included cardiovascular disease. | Large sample size. Authors hypothesise difference in mortality may be due to increased severity of disease when operated (as routine calcium screening introduced in middle of study period). |
| Ogard et al, 2004 [46] | Retrospective cohort study, patient with PHPT who were managed either conservatively or surgically. | 1,578 | Patients with a diagnosis of PHPT had a significantly increased risk of premature death compared to general population. Lower risk of death from all causes in women who underwent surgery. Significantly increased mortality for CVD for women treated conservatively. | Patients identified via national register. Increased risk of cancer in PHPT patients. |
| Palmer et al, 1987 [42] | Observational study of patients with PHPT who had undergone parathyroidectomy; 22-year follow-up | 441 | Higher mortality postoperatively than general population. | Long follow-up period. Historical study, therefore, caution should be applied if extrapolating these results to current surgical practice. |
| Uden et al, 1990 [43] | Multi-center retrospective case control study, long-term follow-up of patients with PHPT who had undergone parathyroidectomy and matched controls. | 282 | Increased mortality in patients who had undergone parathyroidectomy (survival reduced by 18%). Only 1% operative mortality. | Multi-center study, large sample size. Historical study, therefore, caution should be applied if extrapolating these results to current surgical practice. |
| Wermers et al, 1998 [11] | Retrospective cohort study; patients with confirmed PHPT or hypercalcemia of unknown cause. | 435 | 29% underwent parathyroidectomy. Patients with higher serum calcium levels had an increased risk of death. Conservative patients had a non-significant trend towards decreased survival. | Large sample group. Long follow-up period. Majority of patients were white. |