| Journal of Endocrinology and Metabolism, ISSN 1923-2861 print, 1923-287X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Endocrinol Metab and Elmer Press Inc |
| Journal website https://www.jofem.org |
Case Report
Volume 10, Number 3-4, August 2020, pages 110-112
Subacute Thyroiditis in the Course of Coronavirus Disease 2019: A Case Report
Mehmet Guven
Department of Endocrinology and Metabolism, Sirnak State Hospital, Sirnak, Turkey
Manuscript submitted July 25, 2020, accepted August 6, 2020, published online August 26, 2020
Short title: COVID-19 With Subacute Thyroiditis
doi: https://doi.org/10.14740/jem678
| Abstract | ▴Top |
Subacute thyroiditis (SAT) is a non-suppurative thyroid gland inflammation, which usually develops after viral upper respiratory tract infections, accompanied by pain and fever. Here, we present a 49-year-old Turkish man who developed SAT 10 days after the diagnosis of coronavirus disease 2019 (COVID-19). After the COVID-19 outbreak, affecting millions of people worldwide, millions of people are also likely to develop SAT. Therefore, clinicians should pay attention to the development of SAT after COVID-19.
Keywords: Coronavirus disease 2019; Severe acute respiratory syndrome coronavirus 2; Subacute thyroiditis
| Introduction | ▴Top |
Subacute thyroiditis (SAT) is a self-limiting painful thyroid gland disease characterized by acute thyroid gland inflammation secondary to viral infections. SAT usually occurs 2 - 8 weeks after the occurrence of viral upper respiratory tract infection. Thyroid gland pain is generally a symptom that suddenly develops or sometimes becomes more evident. The thyroid gland is large, painful, and tender. It is also frequently associated with viral origin symptoms, such as subfebrile fever, myalgia, arthralgia, weakness, and sore throat.
At the end of 2019, a novel virus emerged in Wuhan, China, which quickly spread across the whole country and even to other countries worldwide, causing a pandemic. In February 2020, the World Health Organization named the cause of the disease as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the disease itself as coronavirus disease 2019 (COVID-19) [1]. Here, we present the case of a 49-year-old patient diagnosed with SAT 10 days after the COVID-19 diagnosis and treatment.
| Case Report | ▴Top |
A 49-year-old male patient without previously known disease presented to the outpatient clinic due to sore throat and fever. His oropharyngeal swab test performed 10 days before presentation due to cough and shortness of breath showed positive for SARS-CoV-2. Unenhanced chest computed tomography (CT) was found to be compatible with COVID-19 (Fig. 1).
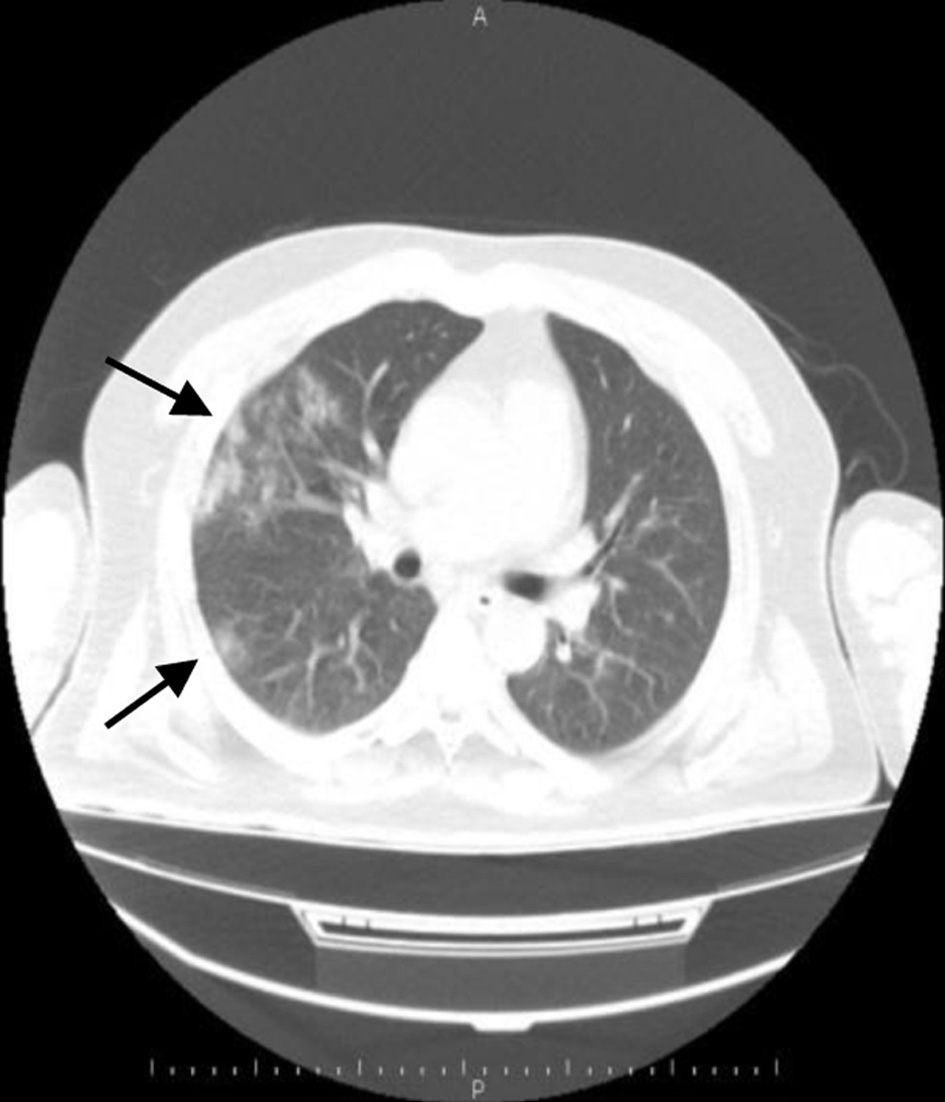 Click for large image | Figure 1. Unenhanced chest CT; the right lung, upper lobe and lower lobe, superior segment reticulonodular density increases, ground glass opacities (arrows). CT: computed tomography. |
Therefore, he was admitted to the infection control facility with the diagnosis of COVID-19 and started 200 mg of hydroxychloroquine twice daily and enoxaparin 0.4 mL once a day. After the treatment, his symptoms improved and discharged. However, he presented to the outpatient clinic 10 days post-discharge due to sore throat, swallowing difficulty, and high fever. Oropharyngeal swab sample was obtained again, showing negative results.
No family members were diagnosed with COVID-19 and no personal history of thyroid disease was observed. He had no contact with the positive case. He did not have a recent travel history. On physical examination, his neck was painful, swollen, and tender by palpation. Tonsils were hyperemic. Other body examinations were normal. His body temperature was 100.94°F (38.3 °C). In the thyroid ultrasound examination, parenchyma is characterized by heterogeneous, patchy infiltrations and hypoechoic areas observed in both thyroid lobes (Fig. 2).
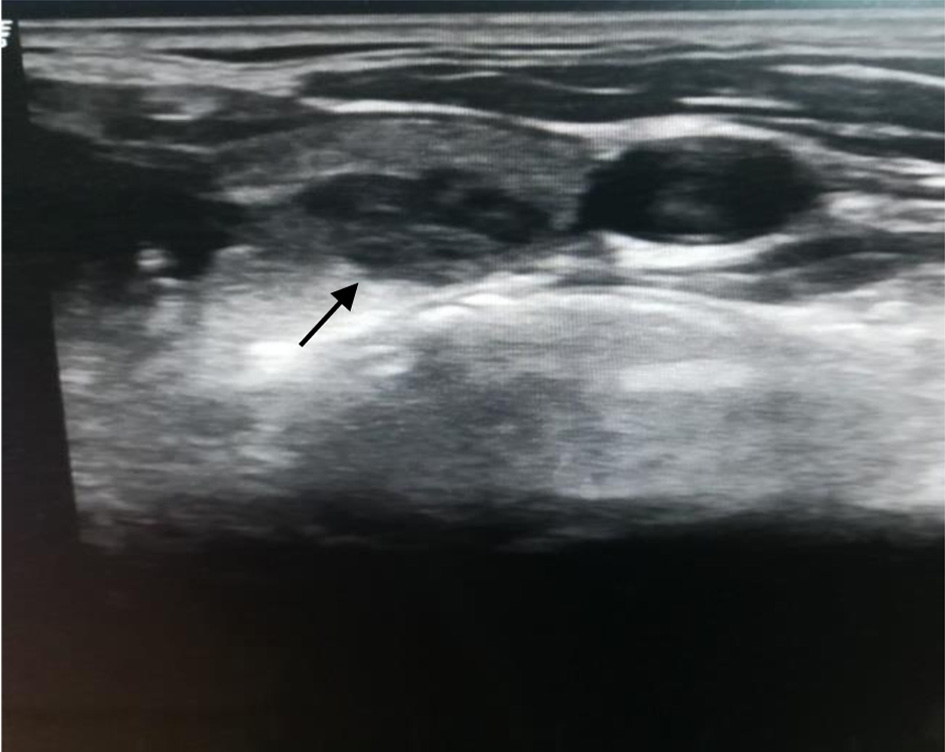 Click for large image | Figure 2. Thyroid ultrasonography (transverse section). Patchy hypoechoic areas in the left lobe (arrow). |
Laboratory examination results are as follows: thyroid-stimulating hormone (TSH)/thyrotropin, < 0.005 µIU/mL; free thyroxine (FT4), 3.61 ng/dL; free triiodothyronine (FT3), 4.24 pg/mL; erythrocyte sedimentation rate (ESR), 80 mm/h; and C-reactive protein (CRP), 7.69 mg/dL. No TSH receptor, anti-thyroglobulin, and anti-thyroid peroxidase antibodies were detected. His blood examination results are shown in Table 1.
 Click to view | Table 1. Blood Results of the Patient |
The patient was diagnosed with SAT, and 32 mg of methylprednisolone was initiated. At 1-week post-treatment, the patient was asymptomatic. Thyroid function and inflammatory markers were lower than the previous values (Table 1). Therefore, the steroid dose was gradually decreased and was planned to be completed in 4 weeks and called for control 1 month after.
| Discussion | ▴Top |
SAT (also known as de Quervain’s thyroiditis or painful thyroiditis) usually occurs following an upper respiratory tract infection (typically after 2 - 8 weeks) and may develop especially due to mumps, measles, coxsackie, influenza, Epstein-Barr virus, human immunodeficiency virus, and adenoviruses [2]. Seasonal summer and transitions support the viral etiology.
Considering the possibility of genetic predisposition and contagious characteristics observed in the same family members, human leukocyte antigen (HLA)-B35-mediated system is thought to play an active role in this mechanism [3].
The characteristic clinical finding of SAT is pain in the thyroid gland that usually starts suddenly or sometimes becomes more evident. Pain may radiate to the neck or jaw area in severe cases and may worsen with neck movements and coughing. Fever, weakness, and fatigue can also be observed due to both inflammation and mild hyperthyroidism. Especially at the beginning period of SAT, palpitations, sweating, and tremors may occur due to high thyroid hormone titers in the blood. These findings usually disappear after 4 - 10 weeks, and the patient may develop asymptomatic, overt, or subclinical hypothyroidism. Our patient complained of sore throat, fever, and difficulty in swallowing. He also had eating difficulty. Despite using a pain reliever tablet, his symptoms remained.
In the laboratory examination, leukocytosis, high CRP, and ESR values (> 50 mm/h) are typical. FT3 and FT4 increased and TSH decreased due to the hormonal release into the circulation from the inflamed thyroid gland. No previous history of thyroid disorder was reported. However, his FT4 level increased and TSH decreased.
In thyroid ultrasonography, large thyroiditis areas were observed in patch style, the patient reported pain during ultrasonography, and the blood flow decreased. He complained of severe pain as soon as the ultrasound probe was placed on his neck while performing ultrasonography. Ultrasonographic images were consistent with the typical SAT diagnosis.
The SAT treatment primarily aimed to reduce pain and tenderness in the thyroid gland. Therefore, nonsteroidal anti-inflammatory drug (NSAID) or prednisone is the preferred anti-inflammatory drug. A 32-mg methylprednisolone tablet was administered daily because of severe sore throat. The patient recovered 2 days post-treatment. Then, after 1 week, the steroid dose was gradually tapered for over 4 weeks, in response to symptom improvement. Thyrotoxicosis spontaneously improved but may be ameliorated with β-adrenergic blockers (such as propranolol); antithyroid drugs play no role for the treatment of SAT during the thyrotoxic phase.
SAT may develop as a result of viral infections or postviral response. The probability of SAT occurrence after viral upper respiratory tract infections increases with COVID-19. Some studies have reported SAT occurrence after viral outbreaks. Other studies also reported that the H1N1 virus, a 2009 pandemic, have caused SAT [4]. Nowadays, studies also reported SAT occurrence after the SARS-CoV-2 infection [5, 6] because many viral agents can cause SAT. SARS-CoV-2 can also be proven as a viral agent that can cause SAT in future research. After the COVID-19 outbreak, affecting millions of people worldwide, millions of people are also likely to develop SAT. Therefore, clinicians should pay attention to the development of SAT after COVID-19.
Conclusions
Clinicians should consider SAT as a late complication of COVID-19 in the future. Delayed diagnosis may result in severe pain. Therefore, early thyroid function tests should be performed in patients with sore throat and fever.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The authors have no conflict of interest to disclose.
Informed Consent
Detailed written informed consent was obtained from the patient.
Author Contributions
This study is entirely author’s own work and no other author contribution.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- World Health Organization. Director-General's remarks at the media briefing on 2019-nCoV on February 11, 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020 (Accessed on February 12, 2020).
- Desaillud R, Hober D. Virus and thyroiditis: an update. Virol J. 2009;6:5.
doi pubmed - Fatourechi V, Aniszewski JP, Fatourechi GZ, Atkinson EJ, Jacobsen SJ. Clinical features and outcome of subacute thyroiditis in an incidence cohort: Olmsted County, Minnesota, study. J Clin Endocrinol Metab. 2003;88(5):2100-2105.
doi pubmed - Dimos G, Pappas G, Akritidis N. Subacute thyroiditis in the course of novel H1N1 influenza infection. Endocrine. 2010;37(3):440-441.
doi pubmed - Brancatella A, Ricci D, Viola N, Sgro D, Santini F, Latrofa F. Subacute thyroiditis after sars-COV-2 infection. J Clin Endocrinol Metab. 2020;105(7).
doi pubmed - Asfuroglu Kalkan E, Ates I. A case of subacute thyroiditis associated with Covid-19 infection. J Endocrinol Invest. 2020;43(8):1173-1174.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Endocrinology and Metabolism is published by Elmer Press Inc.
